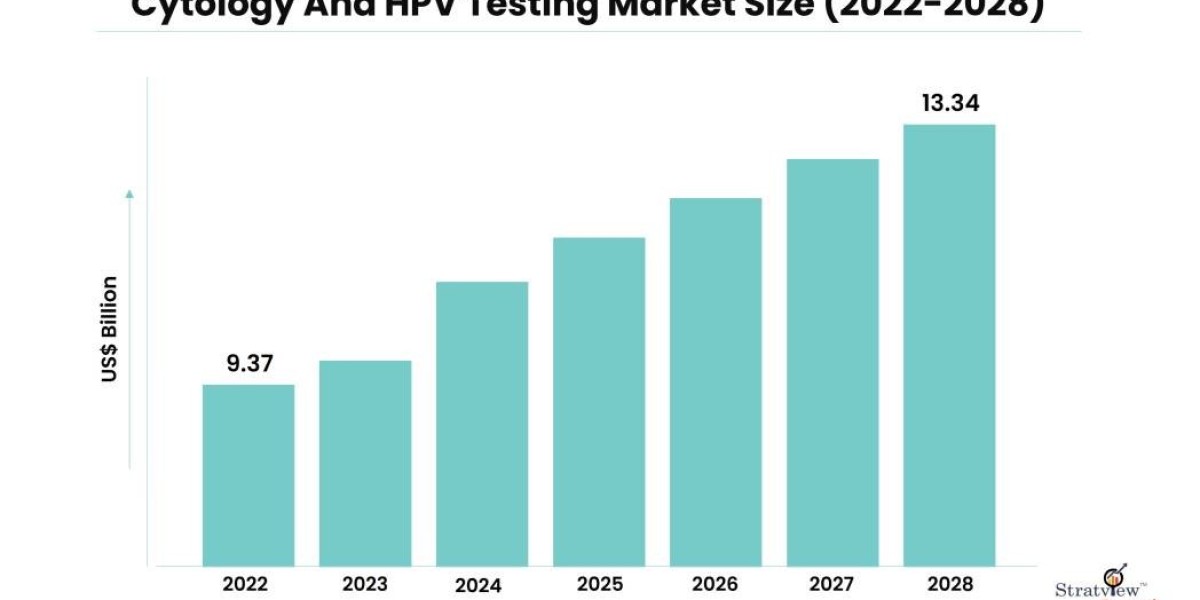
Cervical cancer is a significant health concern worldwide, impacting the lives of millions of women each year. However, the advancement of medical technology has made early detection and prevention more achievable than ever before. Two common screening methods, cytology (commonly known as the Pap test) and HPV testing, play pivotal roles in identifying early signs of cervical abnormalities. In this blog, we will compare the effectiveness of these two approaches and explore their unique advantages in the early detection of cervical cancer. The cytology and HPV testing market is estimated to grow from USD 9.37 billion in 2022 and is likely to grow at a CAGR of 6.0% during 2023-2028 to reach USD 13.34 billion by 2028.
Cytology (Pap Test)
The Pap test has been a cornerstone in cervical cancer screening for several decades. It involves collecting cells from the cervix and examining them under a microscope to identify any abnormal changes in the cervical tissue. The primary goal of the Pap test is to detect precancerous or cancerous cells early, allowing for timely intervention and treatment.
Pros of Cytology:
a. Proven Track Record: The Pap test has been extensively studied and utilized for years, with a long history of successfully detecting cervical abnormalities.
b. Affordable and Widely Available: Pap tests are relatively affordable and accessible, making them feasible in various healthcare settings.
c. High Specificity: The Pap test has a high specificity, meaning it accurately identifies true negative results and minimizes the likelihood of unnecessary follow-up procedures.
Cons of Cytology:
a. Limited Sensitivity: The Pap test's sensitivity is not as high as HPV testing, leading to potential false-negative results and missed opportunities for early detection.
b. Subjectivity: The interpretation of Pap test results depends on the skill and experience of the cytotechnologists, leading to variability in accuracy between different laboratories.
HPV Testing
Human Papillomavirus (HPV) is the primary cause of cervical cancer. HPV testing involves detecting the presence of high-risk HPV DNA in cervical cells. Unlike the Pap test, which identifies cellular changes, HPV testing directly detects the viral infection, thus highlighting the risk of developing cervical cancer.
Pros of HPV Testing:
a. Higher Sensitivity: HPV testing boasts higher sensitivity than cytology, ensuring better detection of high-risk HPV infections and precancerous lesions.
b. Objective Results: HPV testing provides more objective results, reducing the subjectivity seen in cytology interpretation.
c. Better Risk Stratification: The identification of specific high-risk HPV types allows for a more accurate risk stratification, enabling healthcare providers to tailor follow-up procedures accordingly.
Cons of HPV Testing:
a. Higher Costs: HPV testing can be more expensive than the Pap test, potentially limiting its accessibility in certain healthcare settings or regions.
b. Increased Follow-up Interventions: A positive HPV test requires further investigations, including colposcopy and biopsy, which may lead to unnecessary anxiety and discomfort for patients.
Combining Cytology and HPV Testing
Given the unique strengths of both cytology and HPV testing, many healthcare professionals now advocate for a combined approach. Co-testing, which involves performing both tests simultaneously, has shown promising results in various studies.
Benefits of Combined Testing:
a. Improved Sensitivity: Combining both tests results in higher sensitivity, minimizing the chances of false negatives and providing a more comprehensive screening strategy.
b. Better Risk Stratification: Co-testing allows for precise risk stratification by identifying both abnormal cells and the presence of high-risk HPV.
c. Enhanced Efficiency: Co-testing optimizes the screening process, reducing the frequency of unnecessary follow-up procedures and improving overall patient care.
Conclusion
In the early detection of cervical cancer, both cytology and HPV testing play pivotal roles, each offering distinct advantages and limitations. While the Pap test has a long-standing track record and is widely available, its lower sensitivity may result in missed opportunities for early detection. HPV testing, on the other hand, offers higher sensitivity and better risk stratification but comes with increased costs and the need for further investigations.
Combining cytology and HPV testing through co-testing appears to be the most effective approach, as it harnesses the strengths of both methods while mitigating their weaknesses. Ultimately, the decision on which method to employ should be made collaboratively between healthcare providers and patients, considering factors such as age, medical history, and risk factors. Regardless of the screening approach chosen, regular cervical cancer screening remains essential for early detection, ensuring the best possible outcomes for women's health.