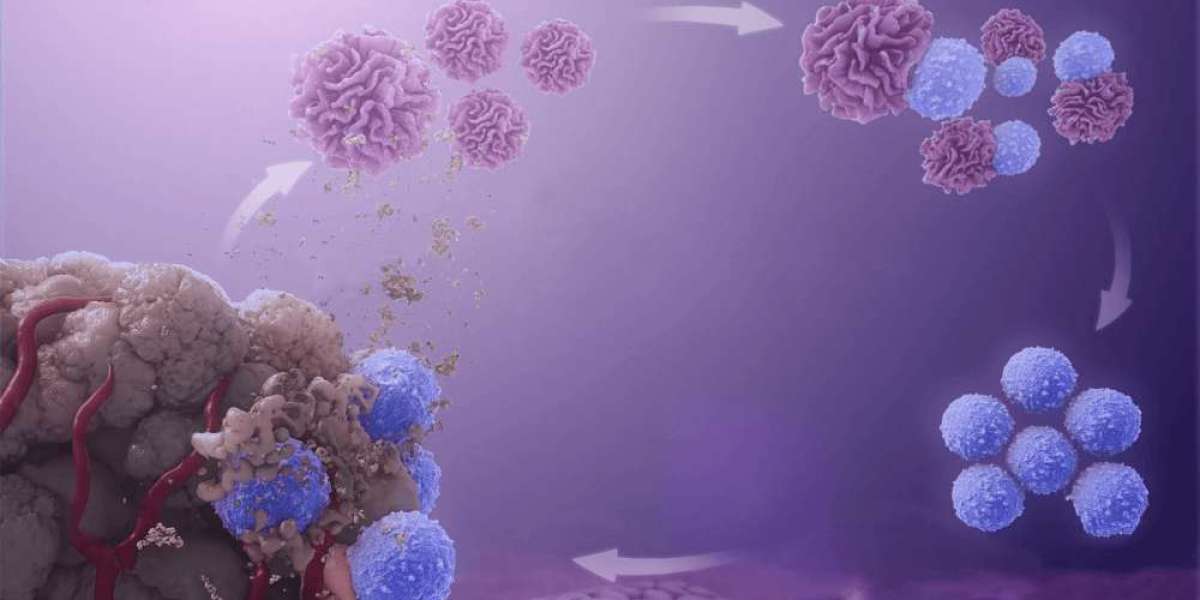
The Autologous Cell Therapy Market is a rapidly growing sector within the broader field of regenerative medicine. This therapy involves using a patient's own cells for treatment, which significantly reduces the risk of immune rejection. It has shown promise in treating a range of diseases, from autoimmune conditions to various cancers and chronic disorders. However, despite the promising potential of autologous cell therapy, there are several challenges that hinder its widespread adoption and commercialization.
1. High Production Costs
One of the primary challenges facing the autologous cell therapy market is the high cost of production. Unlike allogeneic therapies, which use cells from healthy donors, autologous therapies require the collection, processing, and reintroduction of a patient’s own cells. This process is complex and resource-intensive. It often requires specialized facilities, equipment, and skilled personnel to harvest, culture, and modify the cells to suit therapeutic needs.
The patient-specific nature of autologous therapy makes it difficult to scale up production. Every treatment requires an individualized approach, leading to higher manufacturing costs. Moreover, the need for strict compliance with regulatory standards adds further expenses. This makes autologous cell therapies prohibitively expensive for many patients and healthcare systems. Consequently, despite the effectiveness of these therapies, the high price can limit accessibility and prevent widespread adoption.
2. Regulatory Hurdles
Autologous cell therapies are subject to rigorous regulatory scrutiny, which can delay their market entry. Regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) have stringent guidelines for the development, approval, and commercialization of cell-based therapies. These regulations aim to ensure the safety and efficacy of treatments but can also pose significant challenges for manufacturers.
The complexity of autologous therapies, including the need to track and manage patient-specific data, introduces additional layers of regulatory complexity. The regulatory approval process for autologous cell therapy requires thorough clinical trials to demonstrate safety and efficacy, a process that can take years. Moreover, cell-based therapies are often classified as biologics, which means that their development and approval follow a more intricate and time-consuming process than traditional pharmaceuticals.
3. Supply Chain and Logistics Challenges
Autologous cell therapies are inherently dependent on an efficient supply chain. The process of collecting, transporting, and processing a patient’s cells requires careful coordination. Since the cells must be collected from the patient and then transported to a specialized facility for processing, there is an increased risk of delays, contamination, or loss of cell viability during transit.
Additionally, the production process for autologous therapies requires stringent temperature controls and sterile environments to maintain the integrity of the cells. Any deviation in this delicate process can result in the destruction of the cells or a reduction in therapeutic efficacy. The logistics of handling patient-specific materials present significant challenges, particularly when treatments are being delivered to remote or underserved regions where access to specialized medical facilities may be limited.
4. Limited Manufacturing Capacity
The manufacturing capacity for autologous cell therapy remains a bottleneck in the market. Given the highly individualized nature of the treatments, scaling production to meet demand is a difficult task. In comparison to allogeneic therapies, which can be mass-produced and stored for later use, autologous cell therapies require a one-to-one manufacturing process for each patient.
This not only complicates production but also impacts the consistency and quality of the final product. Furthermore, the need for specialized facilities to produce these therapies means that companies must invest heavily in infrastructure. Many organizations are struggling to keep up with demand, leading to long waiting times for patients, and, in some cases, treatment delays.
5. Ethical and Social Concerns
Autologous cell therapies also face ethical challenges, particularly in cases where the therapy involves gene editing or manipulation of the cells. Although autologous therapies use the patient’s own cells, the genetic modification of those cells raises questions about the long-term effects and potential unintended consequences. Concerns over the ethics of gene editing are especially prominent in the context of treating genetic disorders, where modifications may be passed down to future generations.
Additionally, the limited availability of advanced healthcare infrastructure in certain regions raises concerns about access to these therapies. In many countries, particularly in low- and middle-income regions, autologous cell therapies may be inaccessible due to financial barriers, a lack of specialized facilities, and limited healthcare systems. This exacerbates existing healthcare disparities and raises ethical concerns about equity in access to cutting-edge treatments.
6. Cell Quality and Reproducibility
A significant challenge in the autologous cell therapy market is maintaining the quality and reproducibility of the therapy. Since these treatments involve using a patient's own cells, the quality of the cells can vary greatly depending on the individual’s age, health condition, and genetic factors. Variability in the quality of cells can affect the overall success of the treatment.
Moreover, ensuring that the cells behave consistently during the production process is critical for ensuring a predictable and effective outcome. Variations in cell quality can lead to inconsistent therapeutic results, making it difficult to guarantee the effectiveness of the therapy for every patient. Research and technological advancements are essential to overcoming these challenges and standardizing the process.
7. Patient-specific Variability
Lastly, patient-specific variability presents a significant challenge in autologous cell therapy. Since each patient’s cells are unique, the outcomes of autologous therapies can differ widely between individuals. Factors such as the patient’s immune response, the disease being treated, and the biological properties of the cells can all influence how well the therapy works.
Developing personalized therapies that address these variables requires extensive research and a deep understanding of the underlying biology of the patient’s condition. While the approach is highly promising, it also means that the therapies are not one-size-fits-all and must be tailored to each patient’s needs, making the process more complicated and resource-intensive.
Conclusion
The autologous cell therapy market holds immense potential for revolutionizing the treatment of a variety of diseases and conditions. However, the challenges related to production costs, regulatory hurdles, supply chain complexities, manufacturing capacity, ethical concerns, cell quality, and patient variability must be addressed to fully unlock this potential. Ongoing research, technological advancements, and increased investment in infrastructure are key to overcoming these obstacles and ensuring that autologous cell therapies become a viable and accessible treatment option for a broader patient population.