Understanding Osteoporosis-Related Fractures
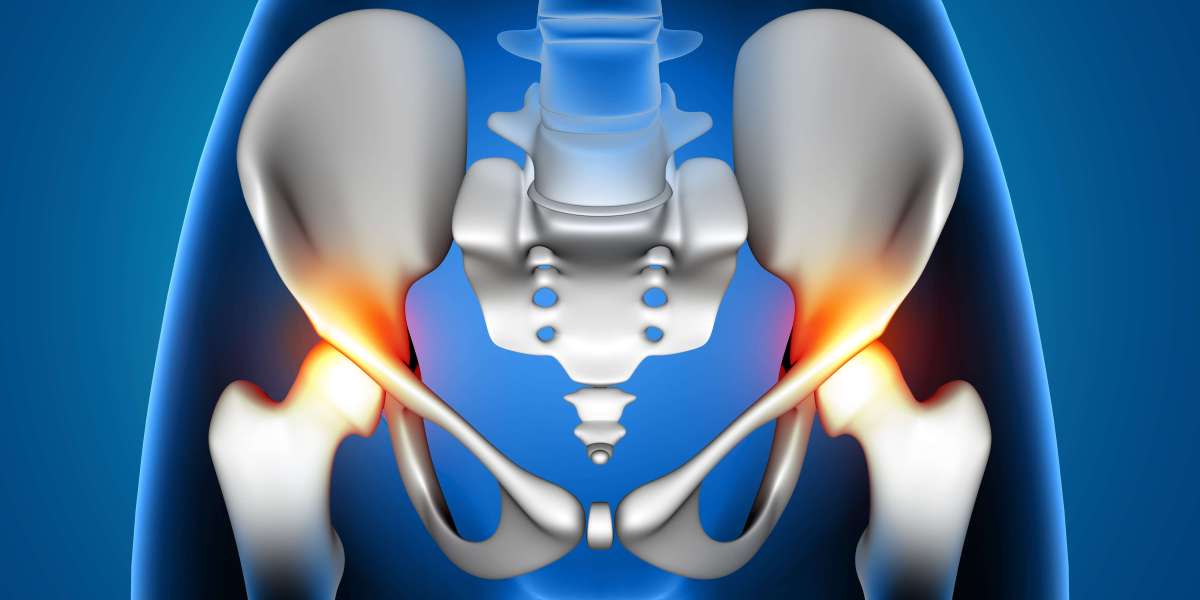
Osteoporosis is a condition where bones become weak and brittle, making them more prone to fractures. Even minor falls, sudden movements, or in some cases, no apparent injury at all can result in fractures. The most commonly affected areas include the spine, hips, and wrists, with spinal fractures being particularly debilitating. However, with early detection and proper management, osteoporosis-related fractures can be prevented.
How Osteoporosis Affects the Spine
Osteoporosis plays a significant role in spinal health. When bones lose density, the vertebrae become fragile and susceptible to fractures, leading to spinal deformities and chronic pain. These fractures can cause:
- Severe back pain
- Loss of height over time
- Development of a hunched posture (kyphosis)
- Reduced mobility and quality of life
In some cases, spinal fractures may not cause significant pain, leading individuals to overlook the condition until it progresses.
Symptoms of Osteoporosis-Related Fractures
The symptoms of osteoporosis-related fractures vary depending on the severity and location of the fracture. Some common signs include:
- Sudden or chronic back pain
- Difficulty standing, walking, or bending
- Height reduction over time
- Visible spinal deformities
- Increased risk of further fractures
Diagnosing Osteoporosis
Early diagnosis is crucial in managing osteoporosis and preventing fractures. The most common diagnostic tool is a Bone Density Scan (DEXA scan), which measures bone mineral density (BMD). The results are given as a T-score:
- Normal: T-score above -1
- Osteopenia (low bone mass): T-score between -1.5 and -2.5
- Osteoporosis: T-score of -2.5 or lower
Additionally, risk assessment tools like the Fracture Risk Assessment Tool (FRAX) help determine an individual's likelihood of fractures in the next 10 years based on factors like age, lifestyle, and medical history.
Risk Factors for Osteoporosis
Several factors can increase the risk of developing osteoporosis and related fractures:
- Age over 65
- Female gender
- Low body mass index (BMI)
- Family history of fractures
- Smoking and excessive alcohol consumption
- Rheumatoid arthritis
- Long-term use of corticosteroids
Treatment Options for Osteoporosis
Osteoporosis treatment focuses on strengthening bones, preventing fractures, and managing pain. The treatment plan may include:
1. Medications
- Bisphosphonates: Alendronate (Fosamax), Zoledronic acid (Reclast) help slow bone loss.
- Denosumab (Prolia): A newer medication that prevents bone breakdown.
- Bone-forming medications: Teriparatide (Forteo) and Abaloparatide (Tymlos) help stimulate new bone growth.
2. Surgical Treatments
For severe spinal fractures causing extreme pain and immobility, surgery may be required:
- Vertebroplasty: A minimally invasive procedure where bone cement is injected into the fractured vertebrae for stability.
- Kyphoplasty: Similar to vertebroplasty but includes the use of a balloon to restore the height of the collapsed vertebra before cement injection.
- Spinal fusion and implants: Required in cases of severe instability.
3. Physiotherapy and Rehabilitation
Physiotherapy plays a key role in osteoporosis management by improving posture, flexibility, and strength. Effective physiotherapy techniques include:
- Myofascial Release: Helps relieve muscle tension around the spine.
- IASTM (Instrument-Assisted Soft Tissue Mobilization): Aids in mobility and pain relief.
- Manual Therapy: Enhances spinal alignment and movement.
- Dry Needling: Alleviates muscular pain linked to fractures.
- Kinesiology Taping: Supports posture correction and movement.
Preventing Osteoporosis-Related Fractures
While osteoporosis-related fractures can be serious, they are preventable with the right lifestyle changes and early intervention. Here’s how you can reduce your risk:
- Maintain a balanced diet: Consume calcium-rich foods like dairy, leafy greens, and fortified cereals.
- Increase Vitamin D intake: Essential for calcium absorption, found in sunlight exposure, fish, and supplements.
- Engage in weight-bearing exercises: Activities like walking, resistance training, and yoga help strengthen bones.
- Avoid smoking and excessive alcohol: These habits weaken bones and increase fracture risk.
- Regular screening: Get a bone density scan if you're at risk, especially after age 50.
Final Thoughts
Osteoporosis-related fractures can significantly impact mobility and quality of life, but with early detection, proper treatment, and preventive measures, the risks can be minimized. Prioritizing bone health through nutrition, exercise, and medical care ensures long-term well-being and independence. If you suspect osteoporosis or have risk factors, consult a healthcare professional for screening and personalized treatment.