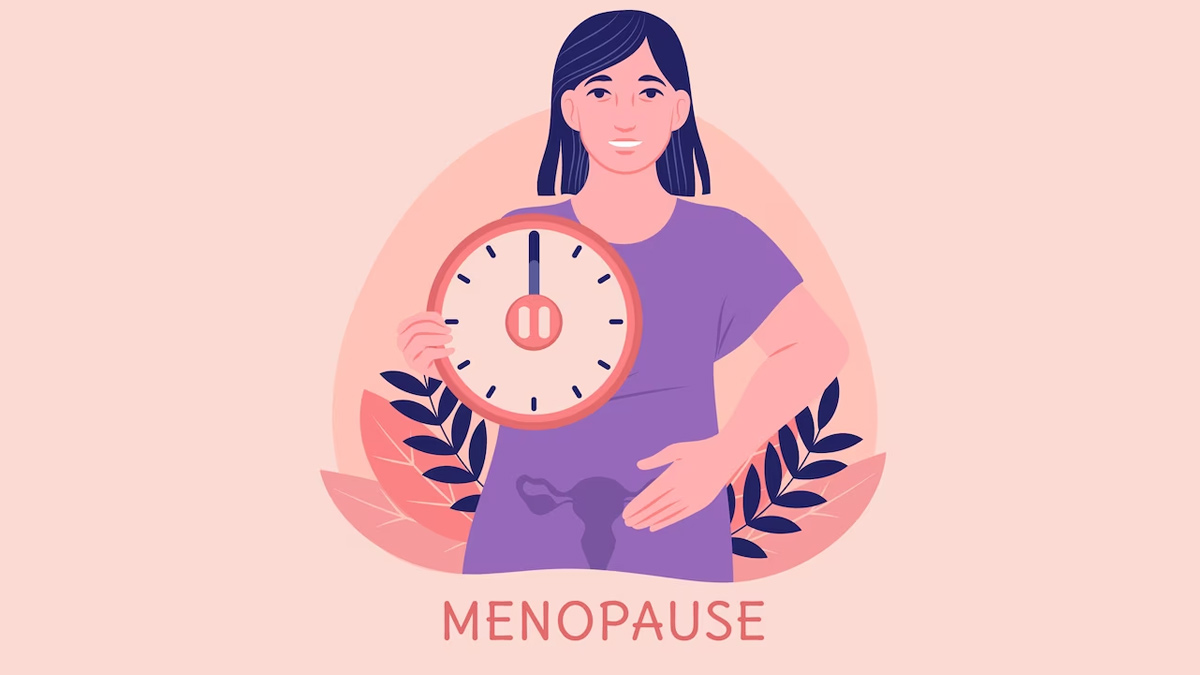
Perimenopause is the transitional phase leading up to menopause, during which a woman’s body undergoes various hormonal changes as it prepares for the end of her reproductive years. This stage typically begins in a woman’s 40s but can start earlier or later. It can last anywhere from a few months to several years.
Common symptoms of perimenopause include:
Irregular menstrual cycles
Hot flashes and night sweats
Mood swings and irritability
Sleep disturbances
Vaginal dryness
Decreased libido
Fatigue
During perimenopause, several hormonal changes occur as a woman’s body transitions from its reproductive years to menopause. The key hormonal changes include:
Estrogen Fluctuations: Estrogen levels become more erratic. Initially, they might fluctuate widely, leading to irregular menstrual cycles. Over time, the overall level of estrogen tends to decline, but this drop is gradual.
Progesterone Decline: Progesterone levels generally decrease as the ovaries produce fewer eggs. This reduction contributes to irregular menstrual cycles and can also affect mood and sleep patterns.
Increased Follicle-Stimulating Hormone (FSH): As the ovaries become less responsive to hormones, the pituitary gland produces more FSH in an attempt to stimulate the ovaries to produce eggs. Elevated FSH levels are often used as an indicator of perimenopause.
Testosterone Changes: Although testosterone levels are lower in women compared to men, they can also fluctuate during perimenopause. Changes in testosterone can affect libido and energy levels.
Changes in Other Hormones: Hormonal balance involves more than just estrogen and progesterone. During perimenopause, there can be changes in other hormones like cortisol (stress hormone) and thyroid hormones, which can also influence overall well-being. It’s essential to look for hormone free solutions that support natural balance.
These hormonal shifts can lead to a variety of symptoms, such as:
Irregular Periods: Cycles may become shorter or longer, and flow may vary.
Hot Flashes and Night Sweats: These are common due to fluctuating estrogen levels.
Mood Swings: Hormonal changes can affect mood, leading to irritability or emotional ups and downs.
Sleep Problems: Difficulty falling or staying asleep can result from night sweats or hormonal changes.
Vaginal Dryness: Declining estrogen can lead to thinning of the vaginal lining, causing vaginal dryness and discomfort. In such cases, using a personal moisturizer can provide much-needed relief by offering hydration and helping to maintain the natural moisture balance of the vaginal area.
Managing these symptoms often involves a combination of lifestyle adjustments, medical treatments, and alternative therapies, tailored to each individual’s needs and preferences.
What can I do to ease the process of perimenopause:
Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help manage symptoms. Foods high in calcium and vitamin D are particularly important for bone health.
Regular Exercise: Engaging in regular physical activity can help manage weight, reduce stress, improve mood, and alleviate some menopausal symptoms like hot flashes.
Stress Management: Techniques such as yoga, meditation, and deep breathing can help manage stress and improve overall well-being.
Adequate Sleep: Establishing a regular sleep routine and creating a comfortable sleep environment can help address sleep disturbances.
Hydration: Staying well-hydrated can help with Intimate dryness and overall health.
Hormone Therapy: Some women find relief from symptoms through hormone replacement therapy (HRT). This should be discussed with a healthcare provider, as it may not be suitable for everyone.
Non-Hormonal Medications: For those who can’t or prefer not to use hormone therapy, certain medications can help manage symptoms like hot flashes and mood swings.
Support Groups: Connecting with other women going through similar experiences can provide emotional support and practical advice.
Regular Check-Ups: Regular visits to a healthcare provider can help monitor symptoms and manage any health issues that arise during perimenopause. Addressing concerns such as vaginal dryness, which is common during this phase, can be easier with the use of products like an intimate moisturizer.
It’s a good idea to consult with a healthcare provider to create a personalized plan based on individual health needs and symptoms.