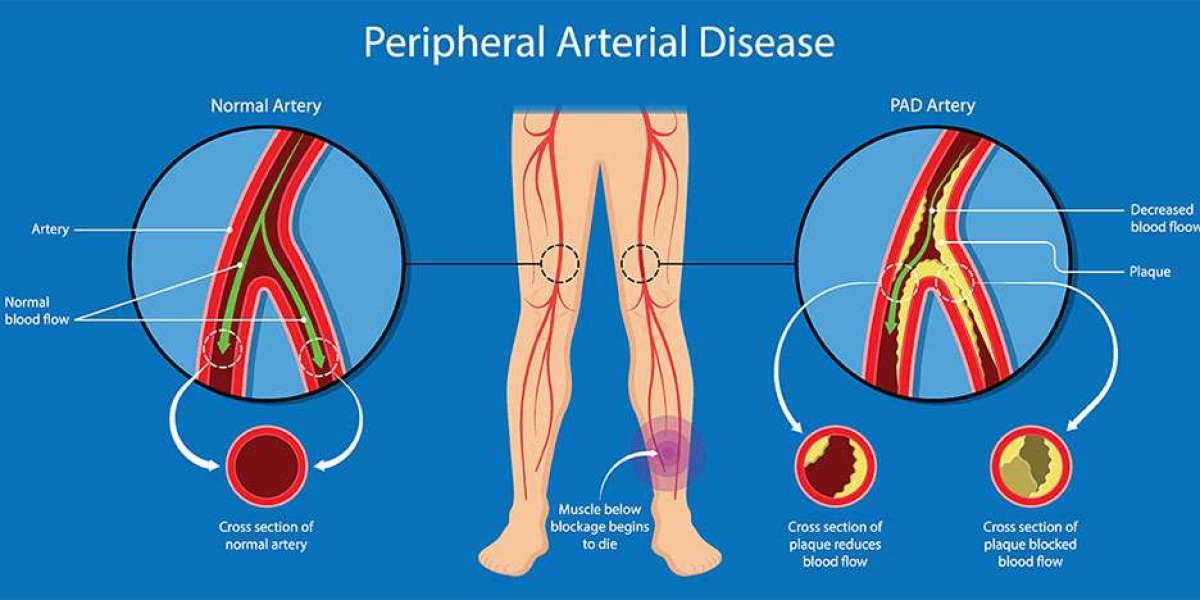
Peripheral Arterial Disease (PAD) is a common circulatory problem where narrowed arteries reduce blood flow to the limbs, particularly the legs. This condition can lead to significant complications, including leg pain, mobility issues, and even amputations in severe cases. Fortunately, treatment for PAD can often be approached through a combination of lifestyle changes and interventional solutions. This article delves into the various treatment options available, emphasizing the importance of a balanced approach to managing this condition.
Understanding Peripheral Arterial Disease (PAD)
What is PAD?
Peripheral Arterial Disease is caused by atherosclerosis, a condition in which fatty deposits (plaques) build up in the arterial walls, narrowing the arteries and reducing blood flow. While PAD primarily affects the legs, it can also indicate widespread atherosclerosis, increasing the risk of heart disease and stroke.
Symptoms of PAD
The symptoms of PAD can vary widely among individuals, but common signs include:
Intermittent Claudication: This is characterized by pain, cramping, or heaviness in the legs or buttocks during physical activities, which typically resolves with rest.
Rest Pain: Pain in the feet or toes while resting, especially at night when lying flat.
Weak or Absent Pulses: Reduced blood flow can lead to weak or absent pulses in the legs and feet.
Leg Ulcers: Non-healing sores or wounds on the feet or legs.
Gangrene: In severe cases, a lack of blood flow can result in tissue death, leading to potential amputation.
Risk Factors for PAD
Several risk factors contribute to the development and progression of PAD, including:
Age: The risk increases with age, particularly in individuals over 50.
Diabetes: Diabetic patients are at higher risk due to potential damage to blood vessels.
Smoking: Tobacco use significantly increases the likelihood of developing PAD.
High Blood Pressure: Hypertension can contribute to arterial damage and narrowing.
High Cholesterol: Elevated cholesterol levels can lead to plaque buildup.
Family History: A family history of cardiovascular diseases may elevate risk.
The Importance of Lifestyle Changes
1. Dietary Modifications
A heart-healthy diet can significantly influence the management of PAD. Here are some dietary recommendations:
Increase Fruits and Vegetables: Aim for a variety of colors and types to maximize nutrient intake.
Whole Grains: Choose whole-grain bread, brown rice, and oatmeal instead of refined grains.
Healthy Fats: Incorporate sources of unsaturated fats, such as avocados, nuts, and olive oil, while reducing saturated and trans fats found in fried foods and processed snacks.
Limit Sodium: Reducing salt intake can help manage blood pressure, a significant risk factor for PAD.
Control Portion Sizes: Keeping an eye on portion sizes can help manage weight, which is crucial for overall cardiovascular health.
2. Regular Physical Activity
Exercise is a cornerstone of PAD management. Regular physical activity can improve circulation, enhance muscle strength, and reduce symptoms. Here are some exercise guidelines:
Supervised Exercise Programs: Participating in a supervised exercise program, such as a walking program, can provide motivation and support while ensuring safety.
Walking: Aim for at least 30 minutes of walking at least three times a week. Start slowly and gradually increase duration and intensity.
Strength Training: Incorporating strength training exercises at least twice a week can help improve overall fitness and manage body weight.
3. Smoking Cessation
Quitting smoking is one of the most impactful changes an individual can make. Smoking significantly worsens PAD and increases the risk of complications. Resources to assist with quitting include:
Nicotine Replacement Therapy: Products like patches, gum, and lozenges can help reduce cravings.
Prescription Medications: Some medications can assist with smoking cessation efforts.
Support Groups: Joining a support group can provide encouragement and accountability.
4. Weight Management
Maintaining a healthy weight is crucial for managing PAD. Excess weight can exacerbate symptoms and lead to additional health issues such as diabetes and hypertension. Strategies for effective weight management include:
Caloric Awareness: Understanding the caloric content of foods can help in making healthier choices.
Regular Monitoring: Tracking weight and body measurements can help maintain motivation.
Consultation with a Dietitian: A registered dietitian can provide personalized dietary plans that cater to individual needs and preferences.
5. Stress Management
Chronic stress can contribute to high blood pressure and poor lifestyle choices. Implementing stress management techniques can improve overall health and well-being. Consider:
Mindfulness and Meditation: Practices that promote relaxation can help manage stress.
Yoga and Tai Chi: These gentle exercises can improve flexibility, strength, and mental health.
Support Networks: Maintaining social connections and seeking support from friends, family, or professionals can alleviate stress.
Interventional Solutions for PAD
In cases where lifestyle changes alone are insufficient to manage PAD, various interventional treatments are available. These procedures aim to restore blood flow to the affected areas.
1. Medications
Several medications can be prescribed to help manage PAD and its symptoms:
Antiplatelet Agents: Medications like aspirin or clopidogrel help prevent blood clots and reduce the risk of heart attacks and strokes.
Statins: These cholesterol-lowering medications can help reduce arterial plaque buildup and improve overall cardiovascular health.
Medications for Claudication: Cilostazol is a medication specifically used to relieve symptoms of intermittent claudication, improving walking distance and quality of life.
2. Angioplasty and Stenting
Angioplasty is a minimally invasive procedure used to open narrowed or blocked arteries. It involves the following steps:
Catheter Insertion: A thin tube (catheter) is inserted into the affected artery through a small incision, typically in the groin or arm.
Balloon Inflation: A small balloon at the catheter's tip is inflated to widen the narrowed section of the artery, improving blood flow.
Stenting: In many cases, a small mesh tube (stent) is placed in the artery to keep it open and prevent re-narrowing.
Benefits of Angioplasty and Stenting:
Minimally invasive with shorter recovery times compared to traditional surgery.
Effective in improving symptoms and restoring blood flow, which can significantly enhance quality of life.
3. Surgical Bypass
In cases of severe PAD, particularly when there is significant blockage, surgical bypass may be necessary. This procedure involves:
Creating a Bypass Route: Surgeons use a graft (which can be a blood vessel from another part of the body or a synthetic tube) to create a new pathway for blood flow around the blocked artery.
Recovery: Recovery from bypass surgery can take longer than other procedures, but it can provide lasting relief from PAD symptoms and improve overall limb health.
4. Endarterectomy
Endarterectomy is a surgical procedure that involves the removal of plaque buildup from the artery wall. It is less common for PAD compared to angioplasty and bypass but may be indicated in specific cases. The procedure typically involves:
Incision: An incision is made in the affected artery to access the plaque.
Plaque Removal: The surgeon carefully removes the plaque to restore blood flow.
Closure: The artery is then closed, often using sutures or grafting techniques.
The Importance of a Multidisciplinary Approach
Peripheral Arterial Disease (PAD) is a complex condition that affects circulation and can lead to serious health complications if left untreated. Due to the multifaceted nature of PAD, effective management often requires a collaborative approach involving various healthcare professionals. This multidisciplinary team works together to address the diverse needs of patients, ensuring comprehensive care that combines lifestyle changes, medical management, and interventional treatments. Below, we detail the roles of each team member and how their collaboration enhances the management of PAD.
1. Primary Care Physicians
Role and Responsibilities
Primary care physicians (PCPs) are typically the first point of contact for patients experiencing symptoms of PAD. They play a crucial role in diagnosing the condition and managing overall health. Their responsibilities include:
Initial Assessment: PCPs evaluate patients for risk factors such as age, diabetes, hypertension, and smoking history. They also assess symptoms like leg pain or ulcers, which may indicate PAD.
Diagnostic Testing: PCPs may order non-invasive tests such as the Ankle-Brachial Index (ABI) or Doppler ultrasound to confirm the diagnosis of PAD and determine its severity.
Treatment Plan Development: Based on the assessment, PCPs create individualized management plans that may include lifestyle modifications, medication prescriptions, and referrals to specialists.
Coordination of Care: PCPs ensure that all aspects of a patient’s health are monitored, coordinating with specialists to manage comorbidities such as diabetes, hypertension, or heart disease.
Ongoing Monitoring: Regular follow-ups are essential to assess the effectiveness of the treatment plan and make necessary adjustments.
Importance
PCPs provide continuity of care and holistic management, ensuring that all aspects of a patient’s health are considered. Their comprehensive approach is essential for early diagnosis and effective management of PAD, reducing the risk of complications.
2. Cardiologists
Role and Responsibilities
Cardiologists specialize in diagnosing and treating heart and vascular diseases, playing a vital role in managing PAD. Their responsibilities include:
Assessment of Cardiovascular Risk: Cardiologists evaluate the overall cardiovascular health of patients with PAD, considering factors like cholesterol levels, blood pressure, and history of heart disease.
Advanced Diagnostic Testing: They may perform specialized tests such as angiography to visualize blood flow in the arteries and identify blockages.
Management of Coexisting Conditions: Cardiologists are skilled in managing comorbidities that often accompany PAD, such as coronary artery disease or heart failure.
Medication Management: They prescribe antiplatelet agents, statins, and other medications to manage symptoms and reduce cardiovascular risks associated with PAD.
Interventional Procedures: In some cases, cardiologists may perform endovascular procedures like angioplasty and stenting to restore blood flow.
Importance
Cardiologists play a critical role in managing the systemic implications of PAD, helping to prevent serious complications such as heart attacks and strokes. Their expertise in cardiovascular health ensures that patients receive comprehensive care tailored to their needs.
3. Vascular Surgeons
Role and Responsibilities
Vascular surgeons are specialised doctors focused on treating disorders of the vascular system, playing a vital role in managing Peripheral Arterial Disease (PAD). Their primary responsibilities include surgicalprocedures to restore blood flow. In severe cases, they perform bypass surgery, creating an alternate blood path using a graft, or an endarterectomy, removing plaque from the artery walls to open up blood flow.
Importance
Vascular surgeons provide specialized surgical care that can significantly improve symptoms and restore blood flow in patients with severe PAD. Their expertise is crucial in cases where lifestyle changes and medical management are insufficient.
4. Intervtenventionl Radiologist
Role and Responsibilities
Interventional Radiologists are highly trained specialists in performing minimally invasive, image-guided procedures to treat vascular diseases, including Peripheral Arterial Disease (PAD). Their key responsibilities include:
Minimally Invasive Techniques: Interventional radiologists use endovascular methods, such as angioplasty and stenting, to restore blood flow in blocked arteries. These procedures are performed through small incisions using catheter-based techniques, providing patients with effective, low-risk alternatives to open surgery.
Preoperative and Postoperative Care: They oversee the entire treatment process, starting with preoperative assessments like Doppler ultrasound and CT angiography to evaluate vascular conditions. Following the procedure, they conduct postoperative follow-ups to monitor healing, address potential complications, and ensure the long-term effectiveness of the treatment.
Patient Education: Interventional radiologists work closely with patients to explain the procedure details, including its benefits and any potential risks. This empowers patients to make informed decisions and take an active role in managing their vascular health.
Importance
Interventional radiologists are essential in managing PAD, offering patients effective, minimally invasive treatments that reduce recovery time and the risk of complications. Their expertise in both endovascular techniques and comprehensive patient care provides a holistic approach, enhancing patients' quality of life and lowering the chances of serious health issues, such as limb amputation, associated with PAD.
5. Dietitians
Role and Responsibilities
Dietitians play a significant role in the management of PAD by addressing nutritional needs and promoting heart-healthy eating habits. Their responsibilities include:
Nutritional Assessment: Dietitians evaluate patients’ dietary habits, weight, and nutritional status to identify areas for improvement.
Personalized Dietary Plans: They create tailored meal plans that focus on reducing risk factors associated with PAD, such as high cholesterol and hypertension. Recommendations may include increasing fruits and vegetables, whole grains, and healthy fats while limiting sodium and saturated fats.
Education on Portion Control: Dietitians provide guidance on portion sizes and food choices to help patients manage their weight, which is essential for overall health and PAD management.
Support for Special Dietary Needs: For patients with diabetes or other conditions, dietitians offer specialized advice to ensure that dietary plans are aligned with their health goals.
Importance
Dietitians contribute to PAD management by promoting healthy eating habits that can help control risk factors and improve overall cardiovascular health. Their expertise is vital in helping patients make sustainable dietary changes that support their treatment plans.
6. Physical Therapists
Role and Responsibilities
Physical therapists (PTs) play an essential role in improving mobility and quality of life for patients with PAD. Their responsibilities include:
Assessment of Mobility and Function: PTs evaluate patients’ physical abilities, including gait, balance, and strength, to develop tailored exercise programs.
Exercise Prescription: They design supervised exercise regimens that focus on improving endurance, strength, and flexibility. Programs often include walking exercises, strength training, and flexibility routines tailored to the patient's abilities and limitations.
Patient Education: PTs educate patients on the importance of regular physical activity, teaching them how to safely incorporate exercise into their daily routines.
Monitoring Progress: They track patients’ progress, adjusting exercise programs as needed to ensure continued improvement and to address any emerging issues.
Importance
Physical therapists are crucial for helping patients with PAD regain mobility and improve their quality of life. Their exercise programs can alleviate symptoms, enhance circulation, and promote overall physical health, complementing other treatment modalities.
Conclusion
Peripheral Arterial Disease (PAD) is a complex condition that requires a comprehensive management approach. By balancing lifestyle changes with interventional solutions, individuals can effectively manage their symptoms, improve their quality of life, and reduce the risk of complications. Emphasizing the importance of a multidisciplinary approach ensures that patients receive holistic care tailored to their specific needs. Whether through dietary modifications, regular exercise, medication management, or surgical interventions, the path to managing PAD is one that requires commitment, education, and support from healthcare professionals and loved ones alike.